Malignant
melanoma more than just a sunburn story? By Dr Chris Barnes, Bangor Scientific and Educational
Consultants October 2013.
E-mail manager@bsec-wales.co.uk Reference list updated March 2015
Abstract
The main types of skin
cancer are briefly reviewed and possible reasons for their increasing prevalence
are raised. A hypothesis is raised that
UV causes malignant melanoma excess risk when there is both vitamin D
deficiency and increased radon gas levels.
Further, public domain mapping for radon gas in the UK is used to
explore the additional hypothesis that vitamin D might offer protection and
further that there is an association of
radon levels not only with squamous cell disease but also with malignant
melanoma. The hypothesis is
convincingly validated. In common with many cancers malignant melanoma cells
exhibit increased oxidative stress, Sander et al 2003. Both UV radiation and nuclear radiation (from
Radon) could be expected to mediate free radical reactions. Vitamin D has antioxidant properties which
will tend to counter reactive oxygen species and products. Relevance for biology, epidemiology and
sunscreen manufacturers is also discussed. Probably all cancers have
co-initiators and co-promoters epidemiologists must start to understand this and
must understand that Bayesian approaches,
even simple, such as here are going to
be the most productive route to outing the truth in this fascinating and
complex realm.
Introduction
Skin cancer falls into
three main categories namely; basal cell carcinoma, squamous cell carcinoma and
malignant melanoma. The first two have
been associated with high doses of UVA and are the most common and least life
threatening types but left untreated they can cause hideous disfigurement. Since sunbeds often have a huge imbalance in
UVA to UVB and have up to double the total UV exposure of the sun they have been associated with an
explosion of all types of skin cancer.
Increases in the more
deadly malignant melanoma which involves the melanin producing cells or
melanocytes were first reported in
Europe in the 1940’s and continue to this day.
Some have blamed the invention of the sunbed, see, for example, Westerdahl et al (1993) (1). Some have blamed the
invention of the ‘foreign’ holiday.
There are some very recent theories that all skin cancers may be caused
by an imbalance in the natural ratios of UVA and UVB, see Maier et al
(2001). To this end, the invention of
sunscreen creams may have accentuated skin cancer and some cream’s contents may
themselves be carcinogenic, Knowland et al 1993 and see
(2). Supporting this is the notion that there is
considerably more sunscreen use amongst young males in Australia than the USA,
see Maclean and Gallagher 1998 (3)
and yet Australia has considerably more Melanoma. Some have even shown an association
with melanoma and the onset of Radio
and TV broadcasting, see Hallberg and Johansson
(2005) (4,), Hallberg
2007 (5) and Hallberg
and Johansson (2011) (6). A limited study in Cornwall has shown an
association of squamous cell cancer with household radon levels, see Wheeler et
al 2012 (7).
Considering all types of
skin cancer, isn’t it is ironic that UVB is essential for the body to
manufacture vitamin D from sunlight. Of
all the countries in Europe, Sweden is perhaps most badly affected by malignant
melanoma. Sun deprived Swedes love
travelling to warmer Mediterranean and
Middle Eastern climes. One has to pose
the question ‘is it their initial lack
of vitamin D make them more susceptible to malignant melanoma?’
Very recently vitamin D
has been branded by some a wonder vitamin with anti-cancer and immune boosting
activity, see for example of several, Garland et al American Journal of Public
Health 2006 (8). Skin cancers have also been associated
with so called ROS (reactive oxygen species) and free radical reactions. UV can of course mediate such reactions as
can nuclear radiation. There are
emerging new theories as to how RFR (non-ionising radio frequency radiation)
might even be able to do the same, see for an example of several, De Luliis et al (2009)
(9) such findings which may indeed give more credulity to the
work of Hallberg and Johannsson for example.
Hypothesis
The
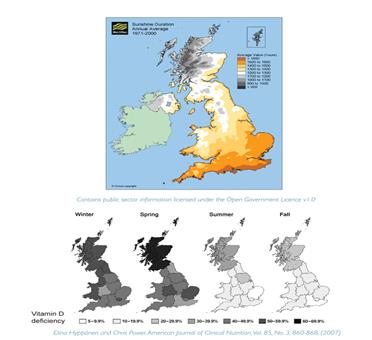
purpose of this study is to use available public domain mapping for sunshine levels firstly to explore
traditional association between UV and malignant melanoma excess risk and
further together with use of mapping for vitamin D deficiency and mapping for
radon to explore the additional hypothesis that vitamin D might offer
protection and further that there may association of radon levels not only with
squamous cell disease but also with malignant melanoma.
Results
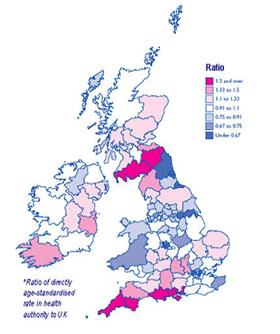
The
results are obtained directly by visual inspection and human visual
meta-analysis interpretation of the mapping data below.
UV
and Malignant Melanoma Assumptions
Making
the assumption that total UVA+UVB will be proportional to sunshine hours, it
can very evidently be seen that there is clearly no simple association between
this quantity and excess risk for the cancer. The latter which is just a high in the
relatively un-sunny Scottish borders and North Lake District region as it is in
the much sunnier Cornwall region. In the
North West Scottish highlands which have least sunshine of all there is lower
cancer risk but not the lowest.
Clearly, then there are other factors at play.
Vitamin
D protection
Some recent studies have
suggested vitamin D might protect from other cancers, especially colorectal,
see Gorham et al (2007) (10). No studies have suggested vitamin D could
protect from malignant melanoma. Thus the findings presented here are entirely
new.
Although not a perfect correlation, it can be seen
that the regions of Britain which have populations with least vitamin D deficiency specifically in Spring seem to correspond with regions which have
much lower malignant melanoma risk, except that is in the South West Midlands.
Radon
another vital factor
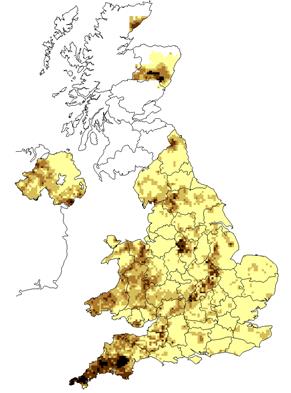
Again not perfect but
spatially very apparent and possibly
significant is that regions of Britain which have high radon concentration s
also seem to have excess risk for malignant melanoma.
Special
cases which test and summarise the overall result and strongly support the
hypothesis
- North
East England –risk minimum =0.67,
vitamin D deficiency least from Spring to Fall, Radon low, UV
Medium/High
- Scottish
borders, risk ratio >1.5 , vitamin D deficiency maximum all year round,
Radon high in West and North East of Region, UV medium
- Cornwall
risk ratio >1.5, vitamin D deficiency medium in winter and spring,
Radon very high, UV High.
- East
Anglia, ratio =1.2, vitamin D deficiency high in spring, Radon Low, UV
High.
- North
West Highlands ratio= 1.0, vitamin D deficiency high all year, UV Low,
Radon Low
- North East Scotland, risk 1.3 , vitamin D
deficiency maximum all year, Radon High in part of region, UV low
- London
risk =.67, vitamin D deficiency lowest in Spring and Fall, Radon low, UV
high
Conclusions
and Further Discussion
The complex hypothesis
appears to have been validated.
Risk of malignant melanoma is minimised
and indeed significantly lower than average
by the protective action of vitamin D in Spring and Fall, irrespective of UV levels in Britain provided Radon exposure is also low.
When vitamin D deficiency extends all
year and radon levels are high there is significant
risk of malignant melanoma even for
regions of Brittan which have low sunshine amounts and hence presumed lower UV
exposure.
Mechanisms
In common with many
cancers malignant melanoma cells exhibit increased oxidative stress, see Sander
et al 2003 (11). Both UV radiation and nuclear radiation (from
Radon) could be expected to mediate free radical reactions. Vitamin D has antioxidant properties which
will tend to counter reactive oxygen species and products.
Relevance
for cancer biology
Associations
have been shown in the past between Radon and non-melanoma cancers
especially squamous cell types but it
is believed this is the first study which shows an association with the more
deadly melanoma type.
The
protective effect of vitamin D is also very relevant for cancer biology in
general.
It has certainly been
shown that melanoma is simply not just a sunburn story.
Relevance
for sunscreen technology
Sun screen creams,
ironically, disturb the balance between UVA and UVB and UVB is essential for
vitamin D formation in the skin. It is
even possible that too much UVA without UVB might promote other problems.
Relevance
for Epidemiology
Because probably all
cancers have co-initiators and co-promoters epidemiologists must start to
understand this and must understand that Bayesian approaches, even simple, such as the above are going to be the most
productive route to outing the truth in this fascinating and complex
realm.
Support
for work of others in the field
This present work lend considerable
independent support to the work Osborne (2002) [12] who stated that there is accumulating evidence that the
vitamin D3/1,25(OH)2D3/VDR axis is important in malignant melanoma (MM) and
importantly that MM cells express the VDR, and the antiproliferative and prodifferentiation
effects of 1,25(OH)2D3 have been shown in cultured melanocytes, MM cells and MM
xenografts. Further very importantly and totally consistent
with the observations here with regard to Spring sunlight Osborne remarks that an
inhibitory effect on the spread of MM cells has been demonstrated and that low
serum levels of 1,25(OH)2D3 have been reported in MM
patients and the VDR polymorphisms have been shown to be associated with both
the occurrence and outcome of MM.
Indeed Osborne goes on to say that further work is
necessary on the influence of serum vitamin D3 levels on the occurrence and
prognosis of MM, the effects of sun protection measures on serum vitamin D3
levels in temperate climates and epidemiological studies on geographical
factors and skin type on the prognosis of MM. In other words he points out the need for
exactly the type of study I have done here.
Finally Osborne
states it would seem mandatory to ensure an adequate vitamin D3 status
if sun exposure were seriously curtailed, certainly in relation to carcinoma of
breast, prostate and colon and probably also MM.
References
- Westerdahl et al
(1993) http://aje.oxfordjournals.org/content/140/8/691.short
- Knowland et al
1993 http://www.sciencedirect.com/science/article/pii/001457939380141G
- Maclean
and Gallagher 1998 http://www.sciencedirect.com/science/article/pii/S0733863505700048
- Hallberg and
Johansson (2005) http://informahealthcare.com/doi/abs/10.1081/JBC-200054260
- Hallberg (2007) http://foodconsumer.org/7777/8888/must-read-news/120907442007_Exclusive_report_Radio_TV_towers_linked_to_increased_risk_of_melanoma.shtml
- http://www.buergerwelle.de/assets/files/hallberg_johansson_2011a.pdf
- http://www.ncbi.nlm.nih.gov/pubmed/22081061
- http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2004.045260
- http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0006446
- Gorham
et al (2007) http://www.sciencedirect.com/science/article/pii/S0749379706004983
- Sander
et al 2003 http://onlinelibrary.wiley.com/doi/10.1046/j.1365-2133.2003.05303.x/abstract;jsessionid=5F5A0701A3159AA65FFCF72BDC887261.f01t02?deniedAccessCustomisedMessage=&userIsAuthenticated=false
- Vitamin
D and systemic cancer: is this relevant to malignant melanoma? J.E. Osborne and P.E. Hutchinson, British Journal of
Dermatology, 147 (2) pp 197-213,
onlinelibrary.wiley.com/doi/10.1046/j.1365-2133.2002.04960.x/pdf