Risk
of Type 2 Diabetes in darker skinned
people and ethnic minorities who have chosen to live in cooler, cloudier
climates far more than just an overweight problem some short comments by
Dr Chris Barnes Bangor Scientific and Educational Consultants, September
2015.
Abstract
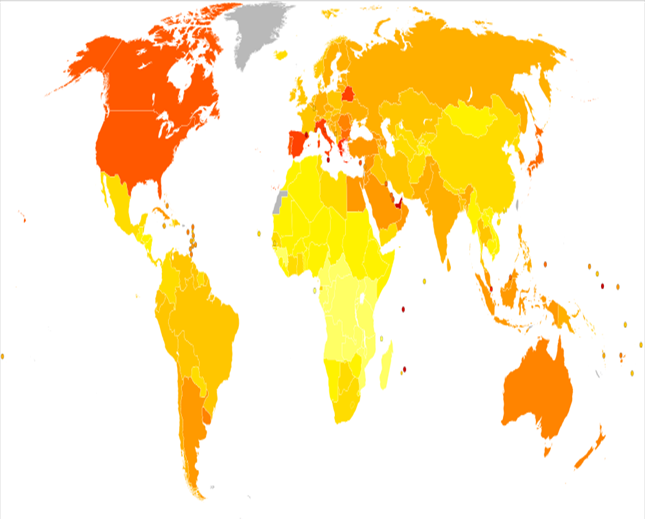
As with certain types of cancer risk, I propose that
poor vitamin D status amongst black and Asian people living in cold cloudy
climates could account for at least some
of their increased type 2 diabetes risk
and renal failure. Quite simply darker
skins designed for protection against bright sunlight do not allow enough
vitamin D production here in the UK. I would expect the problem to be
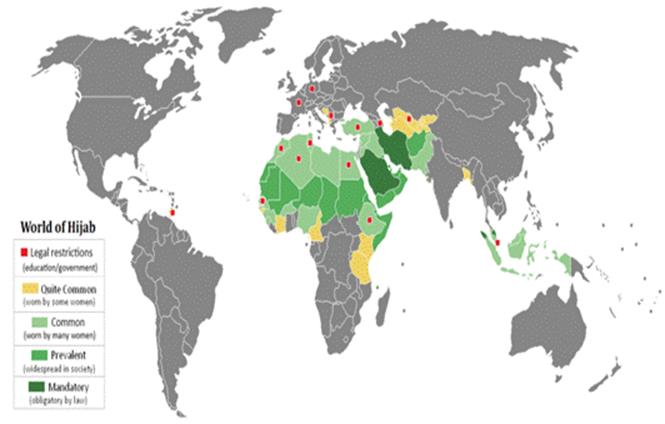
accentuated by Islamic dress. All
parts of the hypothesis are been strongly supported by simple geospatial mapping
considerations. In any event generally
world-wide there appears to be less diabetes in equatorial regions – high solar
UVB. All parts of the hypothesis have
been strongly supported by simple
geospatial considerations.
Introduction
In the USA it is
generally recognised that people of
different racial and ethnic groups are more likely to develop type 2 diabetes,
heart disease, and stroke. African Americans, Mexican Americans, American Indians,
Native Hawaiians, Pacific Islanders and Asian Americans have a higher risk for
these deadly diseases [1,2]. This is partly because these populations are
more likely to be in lower income
brackets, overweight, have high blood pressure the latter possibly a
consequence of their type 2 diabetes.[3].
However,
there is clearly something else at work here because Asians in America also
carry a high type 2 diabetes risk
despite having average BMI’S less than
whites. Lee et al (2011)[4] has also commented on this, stating that additional
investigation of this disparity is warranted, with the aim of tailoring optimal
diabetes prevention strategies to Asian Americans.
Diabetic renal disease
is also more common in patients of Asian
ethnic origin than White Caucasians in the United Kingdom, see Burden (1992/2009)[5]. Dreyer et al (2009) [6] also determined a disparity in the incidence of end-stage renal
failure secondary to diabetes mellitus exists between these ethnic groups. Burden
used a person-time at risk incidence rate for patients receiving renal
replacement therapy secondary to diabetes mellitus in the county of
Leicestershire from 1979 to 1988. The incidence rate of end-stage renal failure
expressed for the estimated population of patients with diabetes mellitus in
patients of Asian ethnic origin was 486.6 (95% CI, 185.1 to 788.1) cases per
million person-years per year, compared to 35.6 (17 to 54.2) in White
Caucasians. All patients of Asian ethnic origin developing end-stage renal
failure had non-insulin-dependent diabetes. The high incidence of end-stage
renal failure secondary to diabetes mellitus in patients of Asian ethnic origin
in the UK imparts significant public health implications for resource planning
and allocation, and the need to initiate strategies to ameliorate renal disease
in this ethnic group.
Hypothesis
As with certain types of
cancer risk, I propose that poor vitamin D status amongst black and Asian
people living in cold cloudy climates could
account for at least some of their increased type 2 diabetes risk and renal failure. Quite simply darker skins designed for
protection against bright sunlight do not allow enough vitamin D production here
in the UK. I would expect the problem to be accentuated by Islamic dress.
Discussion
and Supporting Evidence.
Mohr et al has shown a
strong association between ultraviolet B irradiance, vitamin D status and
incidence rates of Type 1 diabetes in 51 regions worldwide. The lower the U/V irradiance and Vitamin D
status the greater were the type 1 ( congenital ) diabetes incidences. Given this it is not unreasonable to suppose
that type 2 diabetes might be similarly affected. [7]
Wacker and Hollick 2013 [8]
concur elegantly with my hypothesis and state :
‘Vitamin D is the
sunshine vitamin that has been produced on this earth for more than 500 million
years. During exposure to sunlight 7-dehydrocholesterol in the skin absorbs UV
B radiation and is converted to pre-vitamin D3 which in turn isomerizes into
vitamin D3. Pre-vitamin D3 and vitamin D3 also absorb UV B radiation and are
converted into a variety of photoproducts some of which have unique biologic
properties. Sun induced vitamin D synthesis is greatly influenced by season,
time of day, latitude, altitude, air pollution, skin pigmentation, sunscreen
use, passing through glass and plastic, and aging. Vitamin D is metabolized
sequentially in the liver and kidneys into 25-hydroxyvitamin D which is a major
circulating form and 1,25-dihydroxyvitamin D which is the biologically active
form respectively. 1,25-dihydroxyvitamin D plays an important role in
regulating calcium and phosphate metabolism for maintenance of metabolic
functions and for skeletal health. Most cells and organs in the body have a
vitamin D receptor and many cells and organs are able to produce
1,25-dihydroxyvitamin D. As a result 1,25-dihydroxyvitamin D influences a large
number of biologic pathways which may help explain association studies relating
vitamin D deficiency and living at higher latitudes with increased risk for
many chronic diseases including autoimmune diseases, some cancers,
cardiovascular disease, infectious disease, schizophrenia and type 2 diabetes.
A three-part strategy of increasing food fortification programs with vitamin D,
sensible sun exposure recommendations and encouraging ingestion of a vitamin D
supplement when needed should be implemented to prevent global vitamin D
deficiency and its negative health consequences.’
Alqurashi
et al (2011) [9] comment on the
explosion of diabetes in the Saudi community. Clearly
adopting Westernised lifestyles and fast food style diets has not helped and
there is a similar explosion throughout other parts of the Arab world. However most Arabs, particularly in Saudi
Arabia are very heavily clothed and covered from the sun. It is my extended hypothesis that this
accentuates the diabetes in EXACTLY the same way as I have shown elsewhere it
similarly accentuates the problems of hormonal cancers : breast and prostate in
these countries, see Barnes
2013 [10].
Further strong support of
the hypothesis can be gleaned by inspection of the spatial distribution of
diabetes in comparable regions of the world where the hijab is worn and not
worn for example the middle east, Africa and parts of Malaysia, Indonesia and
Papua New Guinea. Saudi Arabia really
stands out in this context. The effect in Papua New Guinea mirrors that for breast cancer [10] and the incidence of type 2 diabetes in 2000 can be seen to be somewhat
higher in the Eastern part of the island
where Hijab wearing is far more common and hence vitamin D status in women
would be expected to be on average significantly lower. Covering up with ,for example, the Hijab is
a warm sunny country seems to produce a
similar diabetes risk to going uncovered
in a cooler, less sunny climate. Thus
the worst possible risk might be expected for those black and Asian Islamic
individuals who migrate to such cooler countries and carry on with their dress
traditions. This may account for the
risk discrepancy observed by unexplained by Lee et al (2011). I have previously proved something similar
for Breast Cancer. However, in the
most developed parts of the world across
the spectrum of races, clearly the effect of obesity and modern technology such
as light at night, TV and computer
screens and wireless technology accounts for the huge excesses in outweighs
these smaller differences. In any event,
generally, world-wide there appears to be less diabetes in equatorial regions –
high solar UVB.
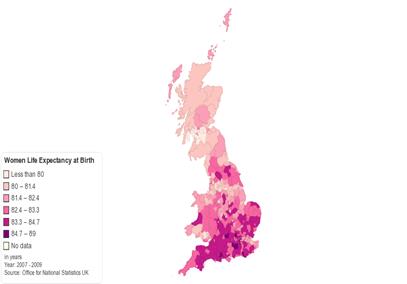
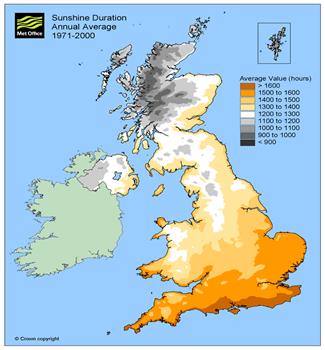
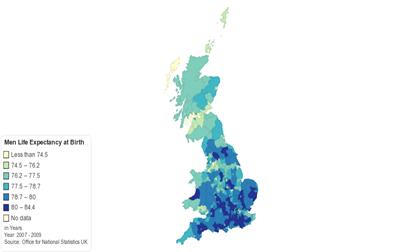
Even here in the UK it would
seem that solar UV in the guise of
sunshine duration is truly and surely the elixir of life. Life expectancy, expected to maximise in
the absence of conditions such as diabetes and cancer, almost completely mirrors sunshine duration in
the below geospatial mapping comparisons.
Conclusions.
All parts of the
hypothesis have been strongly supported by
simple geospatial considerations.
References
1. http://www.diabetes.org/are-you-at-risk/lower-your-risk/nonmodifiables.html
2. Chow et al 2012. http://clinical.diabetesjournals.org/content/30/3/130.full.
3. http://www.diabetes.org/are-you-at-risk/lower-your-risk/nonmodifiables.html
4. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.293.8032&rep=rep1&type=pdf
5. http://www.ncbi.nlm.nih.gov/pubmed/1511571
6. http://qjmed.oxfordjournals.org/content/102/4/261
8. http://www.ncbi.nlm.nih.gov/pubmed/24494042